Is Sclerotherapy Safe? A Step-by-Step Guide to the Sclerotherapy Procedure
Quick Summary
- Sclerotherapy Is Clinically Proven Safe – Used for decades in the U.S. with FDA-approved solutions and a strong safety record when performed by trained vein specialists.
- Minimally Invasive Outpatient Treatment – No surgery, stitches, or general anesthesia required; most patients return to normal activity the same day.
- Step-by-Step Procedure Targets Problem Veins Only–A medical solution is injected into damaged veins, causing them to close and fade while healthy veins take over blood flow.
- Low Risk of Serious Side Effects – Most reactions are mild and temporary, such as light bruising or redness; complications are rare with proper screening.
- Gradual, Natural Results Over Time – The body safely absorbs treated veins, improving leg appearance and circulation without disrupting normal blood flow.
If you’re thinking about treating spider veins or varicose veins, it’s normal to wonder if sclerotherapy is safe and what actually happens during the sclerotherapy procedure. In this guide, we’ll explain how safe sclerotherapy is, how the treatment works, what you can expect before, during, and right after the procedure, the safety measures doctors follow, and how the vein-closing process happens inside your body. By the end of this blog, you’ll clearly understand the full step-by-step process and whether this non-surgical treatment is right for you.

What Is Sclerotherapy?
Sclerotherapy is a minimally invasive medical procedure used to treat spider veins and certain types of varicose veins. A specially formulated solution is injected into the affected vein, causing it to collapse and gradually fade as your body reabsorbs it. Blood is naturally redirected to healthier veins nearby.
This treatment is widely used in the U.S. and is considered one of the safest non-surgical options for vein concerns when performed by trained vein specialists.
Is Sclerotherapy Safe?
Yes, sclerotherapy is safe for most patients when performed by experienced medical professionals. The procedure has been used for decades and is supported by strong clinical evidence. Vein specialists use FDA-approved solutions and precise injection techniques to reduce risks and ensure accuracy.
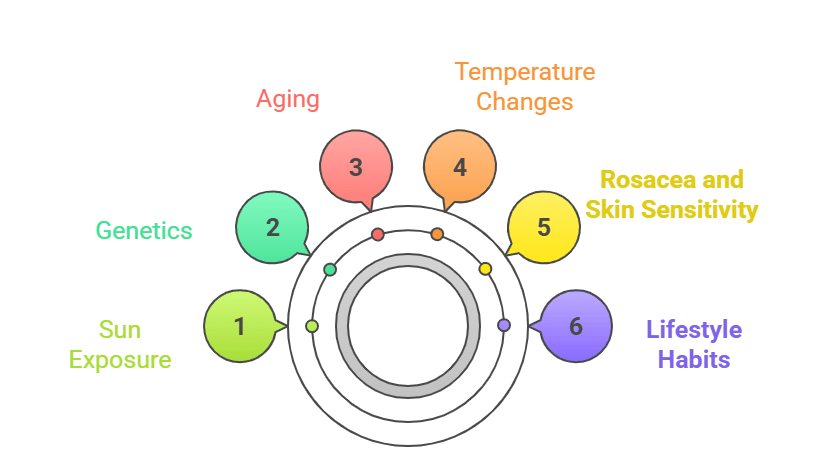
Most people experience only mild, temporary side effects such as slight redness, minor swelling, or light bruising around the injection sites. Serious complications are rare, especially when proper screening is done before treatment. Safety also depends on accurate vein mapping, the correct solution concentration, and careful post-procedure guidance provided by the clinic. You can learn more about how the treatment works and when it’s recommended on our dedicated sclerotherapy treatment service page.
Step-by-Step: The Sclerotherapy Procedure Explained
Here’s a clear, detailed look at what actually happens during the sclerotherapy procedure, from the moment you walk into the clinic to the time you walk out:
1. Pre-Treatment Assessment and Vein Mapping
Before any injections are given, the vein specialist carefully examines your legs. In many cases, a vein imaging test (such as ultrasound) is used to map out the affected veins. This step ensures the doctor treats the right veins and avoids healthy ones. Your medical history is reviewed to confirm sclerotherapy is safe for you and to rule out any potential risks.
2. Skin Preparation and Positioning
You’ll be comfortably positioned, usually lying down with your legs slightly elevated. The skin over the treatment area is cleaned thoroughly to prevent infection. No anesthesia is required because the injections use very fine needles and cause minimal discomfort.
3. Precise Injection of the Sclerosing Solution
The doctor injects a medical solution directly into the targeted vein using a tiny needle. This solution irritates the inner lining of the vein in a controlled way. You might feel a light stinging or tingling sensation for a few seconds, but most patients describe it as very manageable. Each vein is treated individually to ensure accuracy and safety.
4. Immediate Vein Reaction
Once the solution is injected, the treated vein begins to react almost immediately. The vein walls swell and stick together, stopping blood flow through that vein. This is the key part of the procedure, the treated vein is no longer used by your circulatory system, and blood is naturally rerouted to healthier veins nearby.
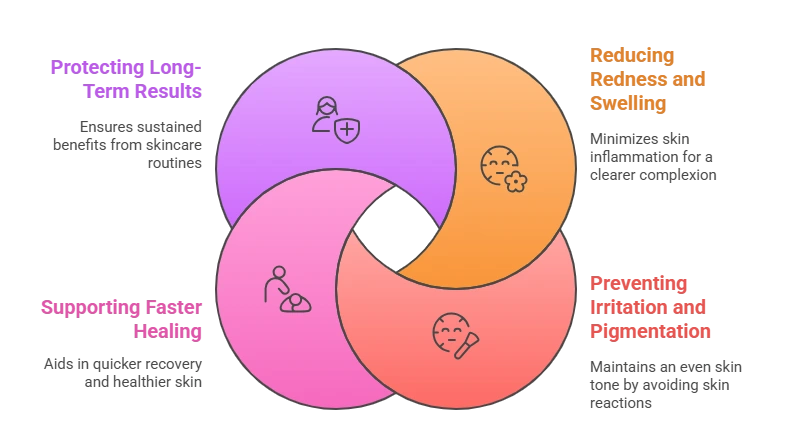
5. Controlled Compression of Treated Areas
After the injections, the specialist may apply gentle pressure or compression to the treated areas. This helps the vein walls stay collapsed and improves the effectiveness of the treatment. In many cases, compression stockings are recommended to support the healing process and improve results.
6. Short Observation and Walk
You’re usually asked to walk for a few minutes right after the procedure. This helps maintain healthy circulation and lowers the risk of complications. Since sclerotherapy is an outpatient procedure, you can go home the same day without downtime.
7. The Body’s Natural Healing Process
Over the following weeks, your body slowly absorbs the closed vein. The vein fades and becomes less visible on the skin’s surface. This natural breakdown process is why results appear gradually rather than instantly. The treated vein does not reopen; instead, it’s replaced by healthier circulation pathways.
This detailed, step-by-step approach is what makes sclerotherapy both effective and safe when performed correctly by experienced vein specialists.
How Sclerotherapy Improves Vein Health Over Time
Beyond cosmetic improvement, the sclerotherapy procedure supports healthier blood flow by redirecting circulation to stronger veins. As treated veins fade, patients often notice their legs feel lighter and more comfortable. This long-term improvement is one of the reasons sclerotherapy continues to be a popular choice across vein clinics in the U.S.
For a deeper look at how sclerotherapy helps with both appearance and comfort, read our detailed guide on the benefits of sclerotherapy for spider veins and varicose veins.
Conclusion:
So, is sclerotherapy safe? When performed by qualified vein specialists using proper techniques, the answer is yes. The sclerotherapy procedure is a proven, minimally invasive treatment that has helped millions of patients in the U.S. improve the appearance and comfort of their legs without surgery.
If you’re considering treatment and want personalized guidance, the best next step is to speak directly with a vein care expert who can evaluate your condition and explain your options clearly. You can schedule a consultation with a specialist through our Contact Us page.
Taking this step can help you move closer to healthier-looking legs and long-term vein care confidence.
.